Pemphigus is a rare, life-threatening skin disorder that affects approximately 1 in 80,000 people worldwide. It is an autoimmune disorder that occurs when the body’s immune system mistakenly attacks healthy skin cells. This results in the formation of blisters and sores on the skin and mucous membranes. Pemphigus can be a very painful and debilitating condition, and can significantly affect a person’s quality of life.
Causes of Pemphigus
There is strong evidence to suggest that genetic factors play a role in the development of pemphigus. Studies have identified certain genetic variations that may increase one’s risk of developing the condition, such as mutations in the genes that encode for different proteins and enzymes that are involved in the production of antibodies. Additionally, familial cases of pemphigus have been identified, which suggests that the condition may be inherited.
Environmental factors may also trigger the development of pemphigus. Exposure to certain chemicals or toxins, such as some medications, insecticides, and solvents, have been linked to the condition. Additionally, certain infections, such as HIV, have been identified as a potential cause of pemphigus.
The cause of pemphigus is believed to be due to an abnormal activity of the immune system. Normally, the immune system produces antibodies to fight off foreign invaders such as bacteria and viruses. However, in individuals with pemphigus, the immune system produces antibodies that attack the skin and mucous membranes, leading to the development of blisters and ulcerations.
Stress can also lead to the development of pemphigus. Stress can trigger changes in the body’s immune system, causing it to produce antibodies that attack the skin and mucous membranes. Additionally, stress can cause changes in the skin, making it more susceptible to the blistering and ulceration associated with pemphigus.
Pemphigus is most commonly seen in individuals over the age of 40, though it can occur at any age. The risk of developing the condition increases with age, likely due to changes in the immune system that occur with aging.
Pemphigus is a complex condition and the exact cause is still not fully understood. However, researchers believe that it is due to a combination of genetic and environmental factors. Additionally, age and stress are believed to play a role in the development of the condition. If you think you may have pemphigus, it is important to speak to your doctor as soon as possible so that you can receive the proper diagnosis and treatment.
Symptoms of Pemphigus
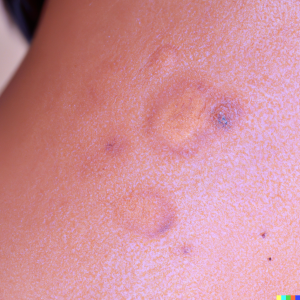
The first symptom of pemphigus is the appearance of blisters or sores on the skin. These blisters usually start out small, but can grow larger over time. They can be very painful and may become itchy or raw. They may also produce a burning sensation when touched. The blisters can appear on any part of the body, but are most common on the face, neck, chest, arms, and legs.
Another symptom of pemphigus is the formation of ulcers on the mucous membranes. These ulcers can form in the mouth, nose, throat, and genitals. They may be painful and may cause difficulty when swallowing or speaking. The ulcers may also ooze cloudy or bloody fluid.
In addition to the skin and mucous membrane symptoms of pemphigus, other symptoms may include fever, chills, fatigue, weakness, weight loss, and joint pain. Pemphigus can also cause problems with the digestive system. Symptoms such as nausea, vomiting, and diarrhea may occur.

Diagnosis of Pemphigus
The first step in diagnosing pemphigus is to take a detailed medical history. A doctor will ask questions about the patient’s medical history, including any prior skin issues, any medications they are currently taking, and any family history of pemphigus. The medical history can help a doctor determine if the patient has a higher risk of developing pemphigus.
The next step is for a doctor to conduct a physical examination. The doctor will look for the tell-tale signs of pemphigus, including blisters, lesions, and other skin changes. The doctor will also take a sample of the blister or lesion to confirm the diagnosis.
The third step is to perform a variety of tests. These tests can help rule out other conditions, such as psoriasis or eczema. Common tests used to diagnose pemphigus include a skin biopsy, an antibody test, and a direct immunofluorescence test.
A skin biopsy is a common method of diagnosing pemphigus. During this procedure, a small piece of skin is removed and examined under a microscope. If a doctor suspects pemphigus, they may ask the patient to take an antibody test. This test checks the patient’s blood for antibodies, which are proteins produced by the immune system when it detects a foreign substance. If a person’s blood contains pemphigus antibodies, it is an indication that pemphigus is present.
The last test used to diagnose pemphigus is a direct immunofluorescence test. During this procedure, a sample of the patient’s skin is taken and examined under a microscope. If pemphigus is present, the skin sample will show signs of the disease, including antibodies.
Prevention and Treatment of Pemphigus
Due to the rarity of pemphigus, there is no single definitive approach to its prevention or treatment. However, there are a number of lifestyle changes that can help reduce the risk of developing the condition and also improve quality of life for those living with pemphigus.
The first step in preventing pemphigus is to avoid triggers. Common triggers include stress, extreme temperatures, certain medications, and certain foods. Avoiding these triggers can help reduce the risk of developing pemphigus. In addition, maintaining a healthy lifestyle is important. Eating a balanced diet, exercising regularly, and getting enough sleep can help keep the immune system functioning properly and reduce the risk of developing pemphigus.
It is also important to take steps to protect the skin from damage. This includes avoiding sun exposure and using sunscreen when necessary. Wearing protective clothing, such as long-sleeved shirts and hats, is also recommended. In addition, avoiding harsh skin care products, such as those containing alcohol or fragrances, can also help protect the skin from damage.
If pemphigus is suspected, it is important to seek medical attention immediately. Early diagnosis and treatment of pemphigus can help reduce the risk of complications and improve the chances of a successful outcome. Treatment typically includes a combination of topical and oral medications. Topical medications, such as steroids and immunosuppressants, can be used to reduce inflammation and prevent blister formation. Oral medications, such as antibiotics, can be used to treat bacterial skin infections. In some cases, ultraviolet light therapy and plasmapheresis (a procedure in which the blood is filtered to remove antibodies) may also be used.
The outlook for people living with pemphigus is generally good with early diagnosis and prompt treatment. While there is no cure for pemphigus, most people are able to manage their symptoms and lead a normal life.